What is Heath Claims Exchange? How does it improve the interoperability of the healthcare ecosystem? How does it help patients improve their insurance claim experience? Lets delve into these questions. But before that, one needs to know why it is important now.
In the recent Arogya Manthan 2022 (programme for celebrating the anniversary of – Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) and Ayushman Bharat Digital Mission (ABDM)) , all the agendas revolved around Universal Health Coverage, bringing stakeholders of digital health together and promoting interoperability in digital health. This is where Health Claims Exchange (HCX) comes into the picture which aims to build an open and interoperable network that can enable health facilities as well as patients to interact with each other in a seamless manner.
Why current health claim process is inefficient?
Our current health ecosystem is fragmented with multiple touchpoints and disaggregated data sets that exist in siloes. This leads to patients lacking a seamless end-to-end digital health experience. This lack becomes a systematic norm and impacts the bottomline of research in the healthcare ecosystem, eventually leading to operational inefficiencies of healthcare providers, TPAs and insurance companies
If you look at the self explanatory Health Insurance Claim Process for Ayushman Bharat, it may look very organized at a superficial level. But each and every step in this process is filled with ambiguity and have a scope of fraud.
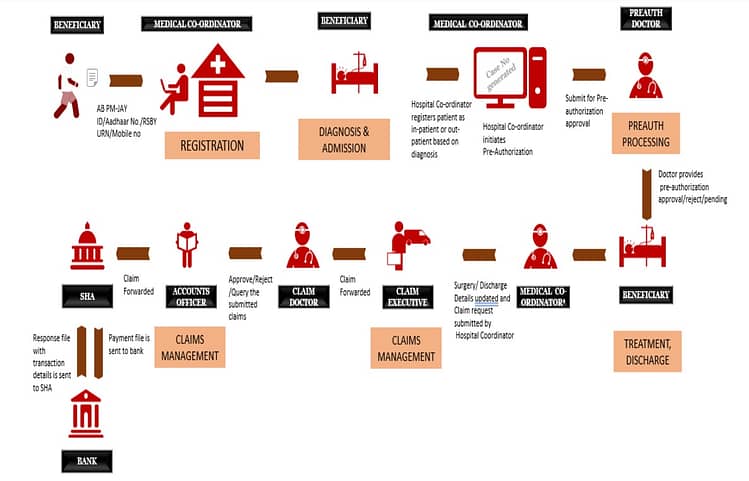
Major challenges of the current process
- Lack of standardization of the claim process across the ecosystem
- Manual entry, emails with images/PDF attachments dictate the data flow
- Insurer, TPA and healthcare provider have their own individual processes
This opaque approach leads to high number of follow ups, high cost of processing the claims, low scalability and poor patient experience. This is where Health Claims Exchange (HCX) becomes important.
What is Health Claims Exchange?
Health Claims Exchange (HCX) is an open source project that aims to define interoperable protocol specifications to enable a multi-party exchange of health claims information. Exchanging claims-related information between various stakeholders – insurers, healthcare providers, beneficiaries, regulatory authority/observers.
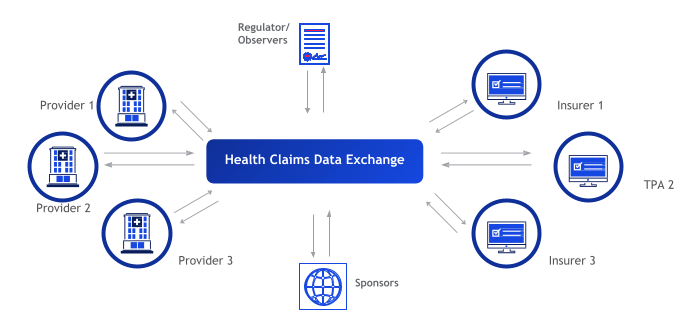
Health Claim Exchange will be initially focused on:
- Standardizing details of healthcare providers (list of procedures covered, cost of the procedures, etc.) and insurers (healthcare providers network, pharmacy network, etc.)
- Checking eligibility of the beneficiary (authentic person, coverage under the insurance, sum insured, etc.)
- Improving pre-auth and claim request flow
- Making payment notification and acknowledgement transparent to all stakeholders
- Increasing accuracy of claim status
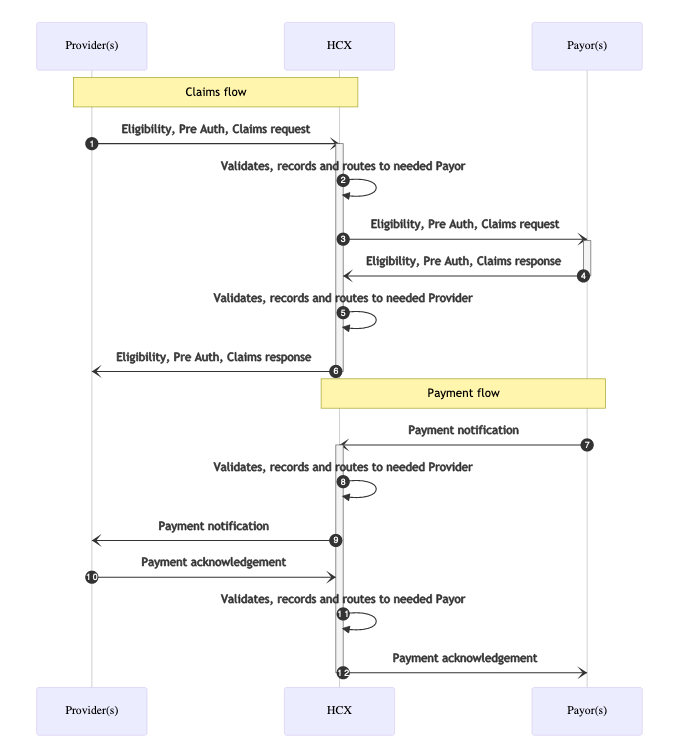
Claim Process with Health Claims Exchange
HCX will take care of validating, recording and routing the message to the relevant stakeholder
Benefits of an interoperable Health Claims Exchange
- Increase in insurance penetration (India’s non-life insurance penetration is just 1% far lower than 8.8% of USA)
- Decrease in cost of claims processing which can enable insurers to focus on new use cases – such as OPD and Pharmacy
- Increase in number of insurers due to decrease in barrier to entry in the insurance business
- Increased adoption of cashless claims model compared to reimbursement
- Personalization in insurance policies with checks for anti-selection
- Increase in low premium micro insurance products
- Better fraud prevention since HCX validates the information
- Standardization of claim process across the country. Currently every policy has its own claim process
- Improved patient experience
HCX on its own will not be disruptive, but with the support of healthcare providers, insurers, TPAs and technology partners, it can be a game changer in the post-COVID world.
Note: In case you are looking for a Product Management course, I would highly recommend joining this cohort-based course – ISB Executive Education – Product Management program
PS: You can connect with me for review or referral discount (link for referral discount)


